- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Why antithrombin is so important
![]()
For someone experiencing thromboembolism, every second counts. Nevertheless, identifying abnormal risk factors potentially causing a thromboembolic event is of no minor importance. Correct diagnosis is critical to identify the underlying cause for changes in antithrombin levels and choosing the right treatment.
What is antithrombin?
Antithrombin (AT) is a natural anticoagulant that is synthesized in the liver. It reduces the activity of thrombin and coagulation factor Xa (FXa), which are responsible for blood coagulation. Even slightly decreased levels of AT can already result in an increased risk of thromboembolic events, like deep vein thrombosis (DVT) or pulmonary embolism (PE)1.
AT forms an irreversible complex with thrombin and factor Xa. Heparin, itself, increases the speed of the complex formation by 1,000 times. AT presence is essential for heparin, both unfractionated and fractionated, to exert its anticoagulatory effect.
When to measure antithrombin in plasma?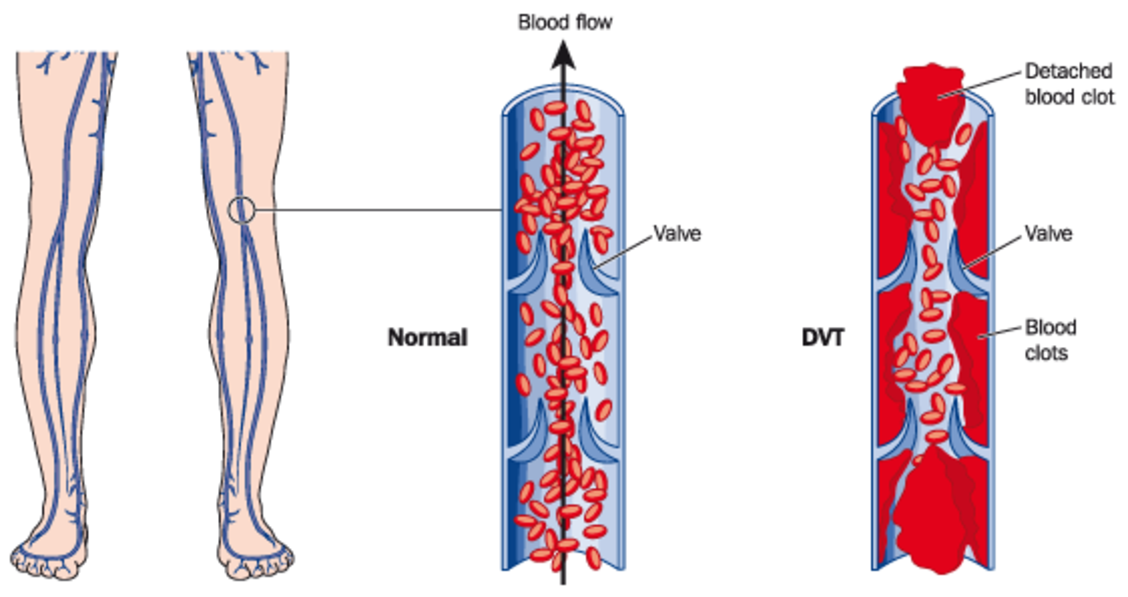
Indications for AT testing can be:
- Screening and diagnosis of antithrombin deficiency
- Recurrent thromboembolic events
- Suspicion of hereditary AT-deficiency
- Suspicion of acquired AT-deficiency
- Monitoring at substitution therapy
- Non-responsiveness to heparin therapy
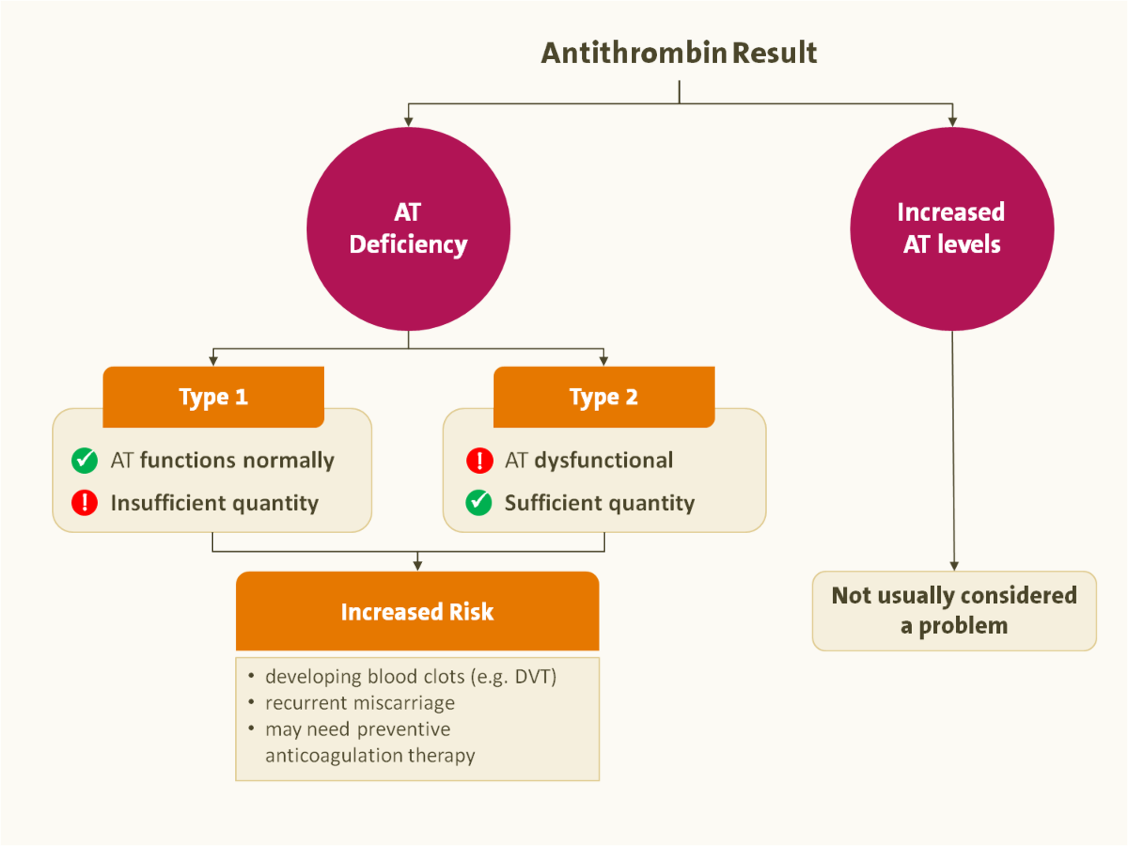
How to interpret AT level results
An inherited (less common) AT deficiency is often associated with thromboembolic disease, and acquired deficiencies (much more common) may occur in liver disease, kidney disease, metastatic cancer and disseminated intravascular coagulation (DIC).
Related Products
The factor Xa-based chromogenic test Hemostat Antithrombinliquid quantifies functionally active AT even at low levels. It has the advantage of being:
- ready to use
- with reagent stability of 21-25 hours
- heparin-insensitive
References
1. Bhakuni, T., et al., Antithrombin III deficiency in Indian patients with deep vein thrombosis: identification of first India based AT variants including a novel point mutation (T280A) that leads to aggregation. PLoS One, 2015. 10(3): p. e0121889.
2. Khor, B. and E.M. Van Cott, Laboratory tests for antithrombin deficiency. Am J Hematol, 2010. 85(12): p. 947-50.
3. Bauer, K.A., T.M. Nguyen-Cao, and J.B. Spears, Issues in the Diagnosis and Management of Hereditary Antithrombin Deficiency. Ann Pharmacother, 2016. 50(9): p. 758-67.
4. Patnaik, M.M. and S. Moll, Inherited antithrombin deficiency: a review. Haemophilia, 2008. 14(6): p. 1229-39.
5. Funk, D.M., Coagulation assays and anticoagulant monitoring. Hematology Am Soc Hematol Educ Program, 2012. 2012: p. 460-5.
6. Thachil, J. and C.H. Toh, Current concepts in the management of disseminated intravascular coagulation. Thromb Res, 2012. 129 Suppl 1: p. S54-9



